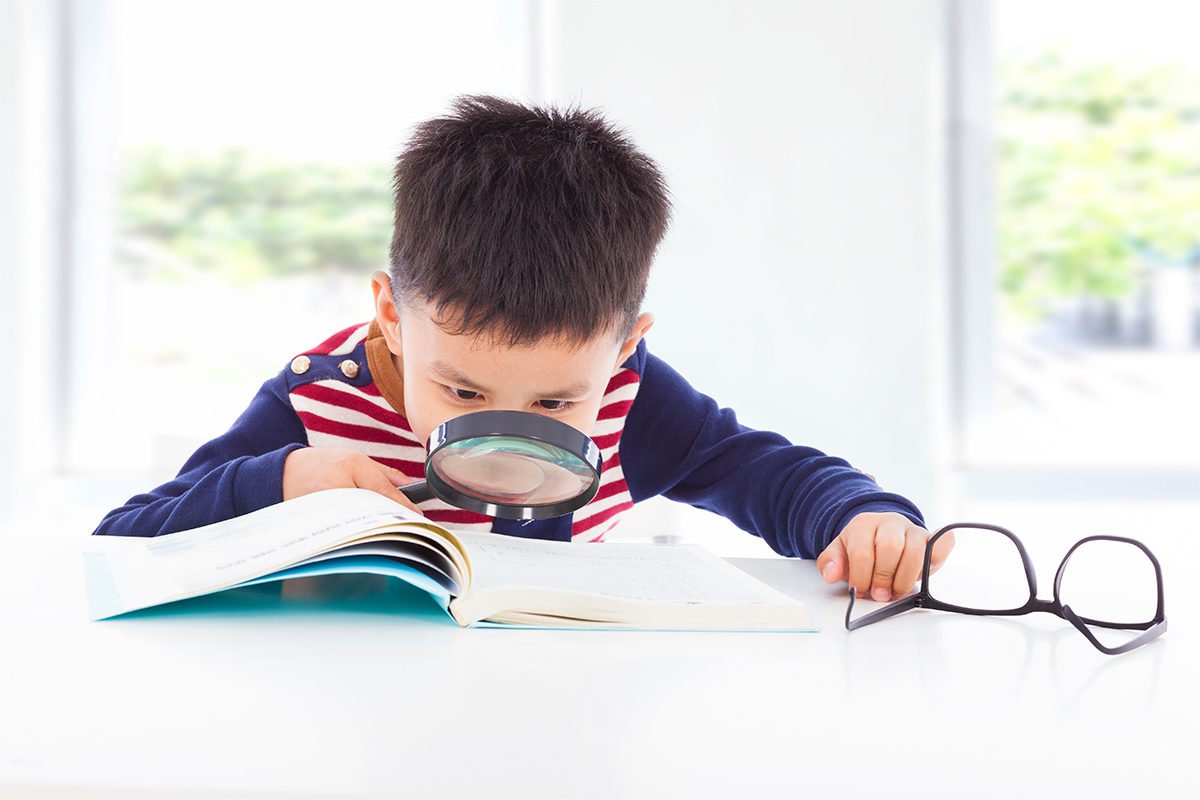
Empowering Young Eyes
Understanding pediatric low vision is crucial for ensuring timely and effective interventions
Pediatric low vision refers to irreversible vision loss or impairment in individuals under 21 years of age. This condition cannot be corrected with refractive measures, medical treatments, or surgical interventions. Specifically, low vision in children is characterised by a best-corrected visual acuity (BCVA) of 20/40 or worse in the better-seeing eye, or a BCVA of 20/30 or worse if accompanied by reduced contrast sensitivity affecting daily tasks like reading, driving, or recognising faces.
Causes Of Pediatric Low Vision
The causes for low vision in children are diverse, ranging from primary ocular structural abnormalities to secondary ocular pathologies. Additionally, low vision may result from genetic or systemic syndromes or cerebral visual impairment (CVI). Common causes include nystagmus, optic atrophy, optic nerve hypoplasia, and CVI.
Structural abnormalities contributing to paediatric low vision include corneal opacification, congenital cataract, primary aphakia, chorioretinal coloboma, and foveal hypoplasia. Ocular pathologies like limbal stem cell deficiency, congenital nystagmus, aniridia, retinal dystrophy, trauma, and iatrogenic damage also play significant roles. Genetic and systemic conditions are major contributors to paediatric low vision.
Recognising Signs
Recognising early signs of low vision in children is crucial for timely intervention. From birth to approximately four months, infants start adjusting to light and focusing on objects. By five to eight months, they develop depth perception and facial recognition. Between nine to twelve months, hand-eye coordination and gross spatial recognition become evident. Delays in these milestones can indicate visual impairment.
Signs of possible visual impairment according to age include:
- Birth-4 months: Decreased sensitivity to bright light, absent or delayed blink reflex, slowed development of a social smile, and nystagmus.
- 5-8 months: Delayed or absent eye contact, failure to fixate on objects or familiar faces, and strabismus.
- 9-24 months: Lack of awareness of own hands, absence of goal-directed hand movements.
- >24 months: Clumsiness with crawling, difficulty reaching toys, holding objects close to the face, problems navigating curbs or steps.
- School-age: Difficulty with reading, complaints of headaches.
As children grow, signs of low vision become more apparent. They may struggle with reading, experience eye strain, or have frequent headaches. These symptoms often lead to misdiagnosis of learning disabilities, emphasising the need for comprehensive eye exams.
Evaluation
Early referral for low vision assessment is essential. The paediatric low vision exam aims to gather detailed information about the child's visual function and identify the cause of the impairment. The evaluation process includes a thorough history, visual acuity measurement, visual field assessment, contrast sensitivity testing, colour vision testing, and refraction assessment.
A detailed history includes the onset, severity, and progression of symptoms. Family history of visual impairment, impact on daily activities, prior use of low vision aids, and difficulties with near tasks and mobility are crucial components.
Visual Acuity testing must consider the child's age and cognitive ability. Gold standard tests include near and distance logMAR testing using age-appropriate optotypes. Testing methods vary by age group:
- 0-36 months: Teller Acuity Cards.
- 4-7 years: LEA symbols, Landolt C, or HOTV optotypes.
- 8-13 years: LogMAR chart.
Visual Field testing in young children involves confrontation visual fields or kinetic perimetry, with standard automated perimetry for older, cooperative children.
Contrast Sensitivity tests like the Hiding Heidi Low Contrast Face Test and Pelli-Robson test provide insights into discrepancies between formal visual acuity and day-to-day functioning.
Colour Vision assessments, including the Ishihara test, Farnsworth D-15 test, or Mollon-Reffin minimalist test, help identify difficulties with object recognition and potential schoolwork challenges.
Cycloplegic Refraction is crucial due to the high incidence of refractive errors in this population. Dynamic retinoscopy prior to cycloplegia evaluates accommodative capacity, guiding the prescription of bifocal corrections if needed.
 Management Strategies
Management Strategies
Managing paediatric low vision requires an interdisciplinary approach involving ophthalmologists, optometrists, occupational therapists, vision rehabilitation therapists, assistive technology trainers, orientation and mobility specialists, psychologists, and vocational counsellors.
Near Vision Aids Children with poor near vision benefit from optical low vision devices like single-vision spectacle magnifiers, hand-held or stand magnifiers, and monocular telescopes. These aids prevent poor posture and neck strain.
Electronic Low Vision Devices Video magnifiers and smartphone applications with voice recognition, screen readers, and audiobooks offer significant assistance. Although video magnifiers provide high magnification, their cost may be prohibitive.
Glare Control and Assistance with Activities of Daily Living (ADLs) Tinted lenses, special absorptive filters, and side shields help manage photophobia. Consistent placement of items at home and school, large print books, adaptive technology, and occupational therapy optimise independence in ADLs.
Psychological Impact And Support
Children with low vision are at higher risk for mental health concerns due to reduced mobility, dependency on caretakers, limited participation in leisure activities, and social isolation. Early detection of mental health issues and social support from family, teachers, and friends are crucial. Professional counselling and promoting self-advocacy from a young age enhance a child's independence and ability to overcome obstacles.
Treatment Outcomes
Early intervention with low vision services leads to improved visual acuity, enhanced visual functioning, better quality of life, and stronger academic performance. Comprehensive low-vision management is essential for achieving these positive outcomes. Evidence supports the benefits of early low-vision rehabilitation, highlighting the importance of timely and appropriate interventions for children with low vision.