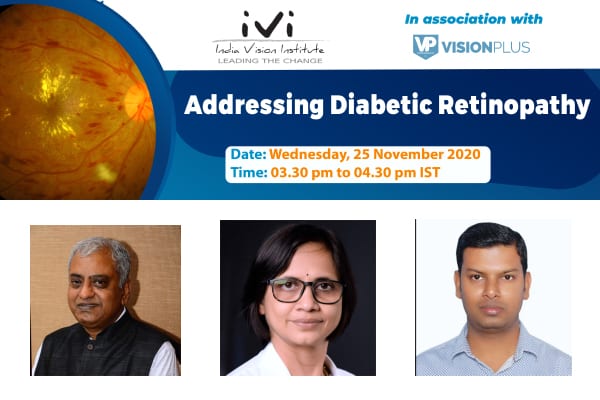
Addressing Diabetic Retinopathy
Diabetic retinopathy, if left unaddressed, may become the leading cause of preventable blindness and visual impairment in India. This pressing challenge has to be addressed by all stakeholders in a concerted and consistent manner. Strategies must aim at building service-delivery capacity and generating awareness, experts say. An estimated 11.9 million people globally may have preventable moderate or severe vision impairment or blindness due to diabetic retinopathy, glaucoma, and trachoma.
As we mark ‘Diabetic Eye Disease Month’ this November, participants at an India Vision Institute (IVI)-VisionPlus Magazine hosted ‘Addressing Diabetic Retinopathy’ webinar, November 25, engaged in an illuminating exchange of ideas and experiences on this emerging challenge. Moderated by IVI’s CEO, Vinod Daniel, the panel at the discussion comprised Prof GVS Murthy, Director, Indian Institute of Public Health, Hyderabad & Professor, Public Health Eye Care and Disability, London School of Hygiene and Tropical Medicine, Dr Padmaja Kumari Rani, Network Head, Tele-Ophthalmology & Consultant, Smt. Kanuri Santamma Retina Vitreous Service, LV Prasad Eye Institute, and Md Alamgir, Optometrist and Founder, Khushi Eye Care.
 Mr Daniel remarked at the outset that diabetes has become a significant health care problem in India and the world. Lifestyle changes related to food habits and a decrease in physical activity, among other factors, have served only to accelerate the rise in diabetes cases the world over. One of the conditions associated with diabetes is diabetic retinopathy, in which high blood sugar levels damage blood vessels in the retina, the nerve layer lining the innermost part of the back of the eye. Vision impairment occurs as a result of swelling in the central part of the retina. Abnormal blood vessels can also grow from the retina, which can result in blindness by causing bleeding or scarring of the retina. The fact that people with diabetes can lose their vision if left unchecked isn’t well known enough, but it is a dangerous possibility.
Mr Daniel remarked at the outset that diabetes has become a significant health care problem in India and the world. Lifestyle changes related to food habits and a decrease in physical activity, among other factors, have served only to accelerate the rise in diabetes cases the world over. One of the conditions associated with diabetes is diabetic retinopathy, in which high blood sugar levels damage blood vessels in the retina, the nerve layer lining the innermost part of the back of the eye. Vision impairment occurs as a result of swelling in the central part of the retina. Abnormal blood vessels can also grow from the retina, which can result in blindness by causing bleeding or scarring of the retina. The fact that people with diabetes can lose their vision if left unchecked isn’t well known enough, but it is a dangerous possibility.
Epidemiological studies have shown that as many as one-third of all people above the age of 40 may have diabetes. Among them, one in five may have some form of diabetic retinopathy. Vision-threatening diabetic retinopathy, which includes diabetic macular oedema and also proliferative diabetic retinopathy, may affect around 10% of them. “Diabetic retinopathy is a problem both in urban and rural India and can affect people from all socioeconomic classes,” said Dr Padmaja Kumari Rani. According to the World Diabetes Report, 2019, an estimated 77 million people in India have diabetes, and a large number of people living with the disease only become aware when they develop complications. A person who develops diabetes will have the condition for life. Accordingly, Prof GVS Murthy suggested that the term “people living with diabetes” be preferred over “patients.”
The need is for an integrated, comprehensive service-delivery model for diabetic eye disease in general and diabetic retinopathy in particular. Coordination between optometrists, ophthalmologists, general physicians, and specialists in multiple medical fields will go a long way in ensuring correct diagnosis and optimum treatment. “A life-long condition like diabetes needs to be managed efficiently, and a one-stop intervention where all services can be provided at one location is important,” noted Prof GVS Murthy. General physicians can play a pivotal role if adequately skilled and equipped to diagnose all diabetes-related complications, including retinopathy, because it will do away with the need for patients to consult multiple specialists.
Most people with diabetic retinopathy in India learn of their condition only after they have lost some vision because of the failure to identify the problem at an early stage. To tackle this, Prof GVS Murthy suggests that every person with diabetes who comes for care to a general physician should, at the very least, have the fundus seen by the physician. “Visual acuity testing and fundus imaging should become part and parcel of a physician’s clinic,” Dr Padmaja Kumari Rani said, echoing Prof Murthy’s assessment. Equipping and skilling general physicians to become anchors of the system will ensure that the most vulnerable sections of society are brought within reach of diabetes-related healthcare services.
Optometrists are uniquely placed to contribute to a comprehensive service-delivery model for diabetic retinopathy. “On average, a patient spends more time with the optometrist than with specialists. Optometrists, therefore, need to be in a position to diagnose diabetic retinopathy and reduce the risk of vision loss by providing comprehensive and timely eye examinations,” observed Md Alamgir. Educating patients, accurately recording patient history, and using retinal tele-screening technology for fundus imaging can be areas of special focus for optometrists going forward.
When general physicians, nursing staff, and optometrists have the requisite skills and equipment, they can act as force multipliers in the system and help manage diabetes and diabetic retinopathy. This, in turn, will pave the way for ophthalmologists to concentrate on treatment instead of having to expend resources on running screening camps. Greater teamwork between optometrists, nursing staff, general physicians, ophthalmologists, and public health professionals is vital.
Improving service-delivery is one part of solving the puzzle. Equally important is advocacy and spreading awareness in the public at large, for which different strategies need to be used depending on the target audience. Mr Daniel asked the panelists to shed light on the significance of this aspect. Dr Padmaja Kumari Rani argued that awareness campaigns featuring public figures such as film stars are highly effective in drawing public attention in many parts of the country.
Awareness campaigns cannot be a stand-alone effort, there needs to be a coordinated, concerted and consistent endeavour to spread awareness and to ensure that the message stays in the minds of the people. The sustainability of awareness campaigns was an issue Prof Murthy alluded to. He outlined the need to be persistent with awareness campaigns because of the lifelong nature of diabetes, which necessitates constant public messaging to remind people of the dangers of diabetes.
Non-governmental organizations (NGOs) are crucial stakeholders and can be game-changers, both in capacity-building for service-delivery and in enhancing public awareness. Responding to Mr Daniel’s question on the room for NGO action, Dr Padmaja Kumari Rani cited the example of the role NGOs played in service delivery and advocacy for cataract blindness in India and stressed on the need for similar efforts in combating diabetic retinopathy.
Different NGOs can contribute in unique ways. The formal NGO sector can, for example, leverage its scale to enhance capacity and advocate for better policy interventions by governments. Small-scale, community-level civil society groups can, at the same time, work at the grassroots level to empower communities and facilitate access to better healthcare.
Living with and managing diabetes is the shared responsibility of multiple stakeholders. Medical practitioners, eyecare professionals and NGOs must come up with integrated approaches at all levels to face the daunting challenges diabetes and diabetic retinopathy will pose in the future.