Five treatment options for Keratoconus
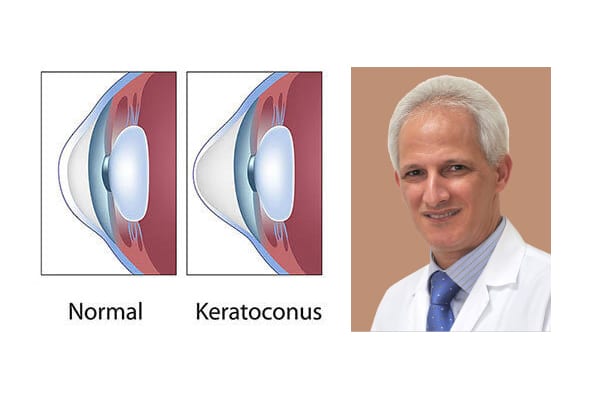
The word Keratoconus comes from two Greek words: kerato (cornea) and konos (cone). Keratoconus is a degenerative disorder of the eye in which the shape of the cornea, which is usually round, is distorted and develops a cone-shaped bulge, resulting in reduced vision.
Keratoconus is a relatively common condition. It affects one person in two thousand, occurs around the world and is quite common in the Middle East. Corneal keratoconus usually affects both eyes asymmetrically, and usually occurs in people between the ages of 10 to 25 years. The condition may progress for 10 years or more and then slow down or stabilize. As the condition progresses, vision becomes distorted and blurred, with increased sensitivity to light and glare.
Keratoconus presents itself in more certain ethnic groups, such as the Arab countries, southern Europe, and southern Asia. Environmental and genetic factors are potential causes, but the exact cause is uncertain. It can be associated with other allergic diseases such as hay fever, eczema and asthma but we are not born with it and its onset usually happens around puberty. It is strongly associated with eye rubbing which can also make the symptoms progress rapidly. It is also seen more common among contact lens wearers.
Treatment options of Keratoconus
The early detection of Keratoconus can have a significant impact on the success of treatment protocol. In fact, early detection is possible by generating computerized corneal shape and thickness measurements through corneal topography, using advanced technology such as a pentacam machine. If left untreated, Keratoconus could lead to significant visual impairment and blindness. Some of the most successful treatment options include:
1- Spectacles and (Hard, Scleral or Toric Implantable) Contact Lenses
These can provide good vision in the early stages of the condition and usually help to correct myopic astigmatism. When spectacles don’t work, rigid contact lenses and Scleral lenses usually provide very good vision if the patient can tolerate them. However, they should be fitted by a contact lens specialist.
Toric Implantable Contact Lenses are generally used to treat high myopic astigmatism in patient who can see well with glasses. But if vision with glasses not good it may be used after improving corneal shape with an intracorneal ring or with very limited therapeutic Eximer laser correction. It can eliminate the need for optical aids altogether and in some patient’s results in improved vision and balance between the two eyes.
2- Corneal Collagen Cross linking (CXL) with Riboflavin (Vitamin B2)
This technique increases the strength of the cornea and prevents the progression of Keratoconus. The modern approach of accelerated pulsed crosslinking is used to ensure an easier procedure for the patient. We use ultraviolet A (UVA 360 nm), Riboflavin (vitamin B2) to stiffen and harden the cornea about four times and this stops the deterioration of keratoconus. The process is carried out under topical anaesthesia and several drops of riboflavin are placed in the eye for about 15 minutes and activated by ultraviolet (UVA) rays ranges from eight to thirty minutes depend on the case. The corneal cross linkage is considered one of the safest and most successful operations used to stop keratoconus degradation and may lead to some improvement in some cases.
3- Intracorneal Rings (Intacs , Keraring or Ferrara ring implants)
These rings inserted into the cornea change the shape of the corneal cone, flattening it and making it a more regular and more central. This will help improve the vision for the majority of patients. We use it when patients cannot tolerate contact lenses, while the cornea is still clear, and the keratoconus condition is not very advanced. A Femto-second laser is used to create the tunnel and the entry point for the rings, which has made it a very safe, affective and reliable procedure.
4- Phototherapeutic Keratectomy (PTK) or Topography-guided laser surgery (TG-PRK)
Keratoconus patients are not candidates for Lasik or normal laser correction. However, some patients benefit from limited PTK using corneal surface eximer laser correction to improve the surface irregularity of the cornea, when contact lenses cannot be tolerated. PTK is always combined with corneal cross linkage, undertaken either during the same procedure or afterwards. Patient should be aware it is not to get rid of the glasses.
5- Corneal transplantation
It is recommended in advanced cases of keratoconus. Out of all types of organ transplant surgeries (heart, lung, and kidney), corneal transplantation is the most widespread and successful of these.
There are various methods used for corneal transplant surgery. The old method includes removing the full thickness of diseased cornea and fixing the healthy cornea with stitches. As for following modern methods, the diseased frontal layers (DALK) is replaced and the patient retains the posterior portion of the cornea, thereby reducing the percentage of corneal transplants complications, especially the rate and severity of the corneal graft rejection.
To conclude, progression of Keratoconus depends on the patient’s age at the time of onset and the severity of eye rubbing. It is very important to avoid eye rubbing as it is also predisposing factor. The earlier the onset, the faster Keratoconus may progress. The condition always affects both eyes differently, so one eye may be more affected than the other. Future treatment for keratoconus is prevention. Molecular genetics are currently being studied and we hope to identify people who are predisposing for the condition to discover early and apply preventive treatment.