This post is also available in:
![]() العربية
العربية

Understanding Keratoconus: A Comprehensive Guide
A discussion on keratoconus with early diagnosis, treatments, and lifestyle adjustments for clarity
Keratoconus is a progressive eye disorder that affects the cornea, the transparent front part of the eye. This condition, though relatively rare, can have a significant impact on a person's vision and quality of life. In this article, we will explore what keratoconus is, its causes, symptoms, diagnosis, treatment options, and how individuals with this condition can manage and cope with the challenges it presents.
What is Keratoconus?
Keratoconus is a non-inflammatory eye disorder that results in the thinning and bulging of the cornea into a cone-like shape. Normally, the cornea has a dome shape, helping to focus light into the eye and onto the retina. However, in individuals with keratoconus, the weakened cornea cannot maintain its shape, leading to distorted vision.
Causes of Keratoconus
The exact cause of keratoconus is not well understood, but a combination of genetic and environmental factors is believed to contribute to its development. Research suggests that individuals with a family history of keratoconus are at a higher risk of developing the condition. Additionally, constant eye-rubbing, poorly fitted contact lenses, and certain conditions like atopic diseases (eczema, hay fever, asthma) may increase the likelihood of keratoconus.
- Family history: If someone in your family has this condition, you have a greater chance of getting it yourself. If you have it, get your children’s eyes checked for signs starting around age 10.
- Age: It usually starts when you’re a teenager. But it might show up earlier in childhood or not until you’re 30. It can also affect people 40 and older, but that’s less common.
- Certain disorders: Studies have found a connection between keratoconus and systemic conditions such as Down syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, and retinitis pigmentosa.
- Inflammation: Inflammation from things like allergies, asthma, or atopic eye disease can break down the tissue of the cornea.
- Eye rubbing: Rubbing your eyes hard over time can break down the cornea. It can also make keratoconus progress faster if you already have it.
- Race: One study of more than 16,000 people with keratoconus found that people who are Black or Latino are roughly 50% more likely to get it than people who are white.
Symptoms of Keratoconus
The symptoms of keratoconus usually begin to manifest in late adolescence or early adulthood. Common signs include:
- Blurred or Distorted Vision: As the cornea bulges and thins, it alters the way light enters the eye, leading to blurry or distorted vision.
- Increased Sensitivity to Light: Individuals with keratoconus often become more sensitive to light, experiencing discomfort even in normal lighting conditions.
- Frequent Changes in Prescription Glasses or Contact Lenses: Due to the progressive nature of keratoconus, individuals may find that their prescription glasses or contact lenses need frequent adjustments to maintain clear vision.
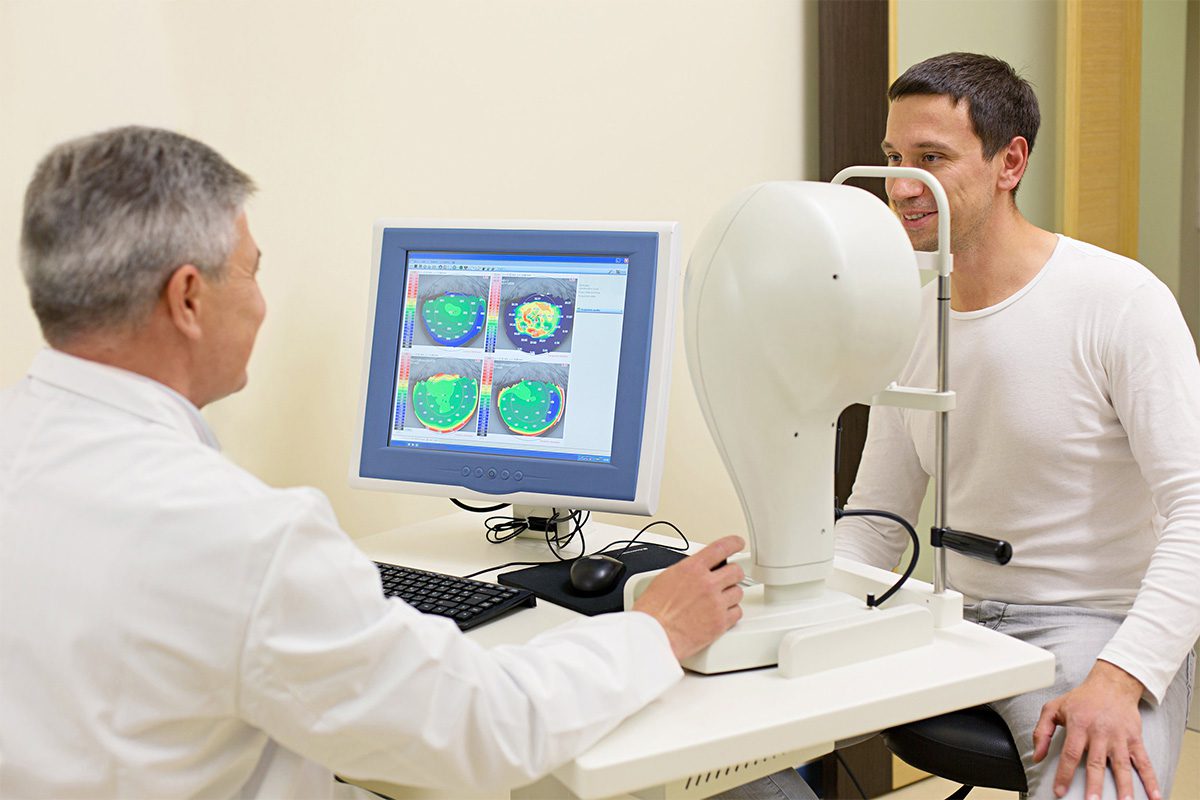
Diagnosis of Keratoconus
Early diagnosis is crucial for effective management of keratoconus. Eye care professionals use various tests to determine the presence and severity of the condition. These tests may include:
- Corneal Topography: This imaging technique creates a detailed map of the cornea's surface, helping to identify irregularities indicative of keratoconus.
- Slit-Lamp Examination: A slit-lamp is used to examine the cornea's structure, allowing for a close inspection of any abnormalities.
- Refraction Test: This test measures the eye's ability to focus light and can reveal the extent of refractive errors caused by keratoconus.
Treatment Options
The treatment approach for keratoconus depends on the severity of the condition. In the early stages, corrective lenses, such as glasses or soft contact lenses, may be sufficient to address mild visual distortions. As the condition progresses, other treatment options may include:
- Rigid Gas Permeable (RGP) Contact Lenses: These specialized lenses provide a smooth surface over the irregular cornea, improving vision by compensating for the distorted shape.
- Corneal Cross-Linking: This minimally invasive procedure involves applying ultraviolet light and a photosensitizing solution to strengthen the corneal collagen, preventing further bulging.
- Intacs: In more advanced cases, small plastic inserts called Intacs may be surgically implanted into the cornea to reshape it and improve vision.
- Corneal Transplant (Penetrating Keratoplasty): In severe cases where other treatments are ineffective, a corneal transplant may be considered. This involves replacing the damaged cornea with a donor cornea.
Living with Keratoconus
While there is no cure for keratoconus, individuals with the condition can take steps to manage their symptoms and improve their quality of life:
- Regular Eye Exams: Routine eye examinations are essential for monitoring the progression of keratoconus and adjusting treatments as needed.
- Eye Hygiene: Avoiding eye rubbing and practicing good eye hygiene can help prevent further damage to the cornea.
- UV Protection: Protecting the eyes from excessive ultraviolet (UV) exposure can help slow the progression of keratoconus. This includes wearing sunglasses with UV protection.
- Support Groups: Joining support groups or seeking counseling can provide emotional support and valuable information for individuals living with keratoconus.
Keratoconus may present challenges, but with early diagnosis and appropriate management, individuals can lead fulfilling lives. Advances in treatment options and ongoing research offer hope for improved outcomes and a better understanding of this complex eye disorder.
If you or someone you know is experiencing symptoms of keratoconus, it is crucial to seek prompt medical attention to ensure timely diagnosis and intervention. Remember, with the right care and support, individuals with keratoconus can navigate the visual challenges and maintain a good quality of life.
American Academy Of Ophthalmology