This post is also available in:
![]()
![]()
![]()
![]()
![]()
![]()


Assessment Of The Tear Film Part 2
In this second part of the 3 part series, we continue from where we left off in the previous article.
Tear film evaluation can be divided into two areas – assessment of tear quantity (volume) and tear quality (stability). Each shall be considered in turn. In this article we will look at the first area - Tear Quantity
Tear Quantity
Bearing in mind that stimulation of reflex tearing will affect any evaluations it is generally suggested to perform the least invasive techniques first. As the bright light source from the slit lamp will inevitably provoke a degree of reflex tearing, it is advisable to perform tear quantity evaluations towards the beginning of the assessment.
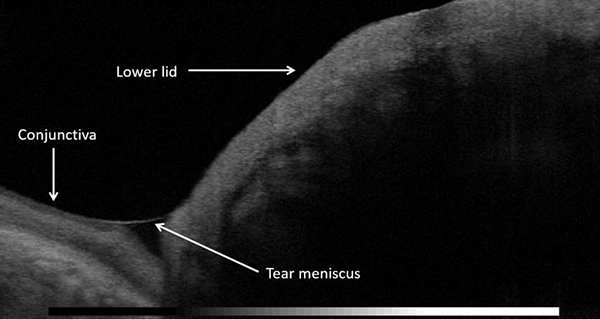
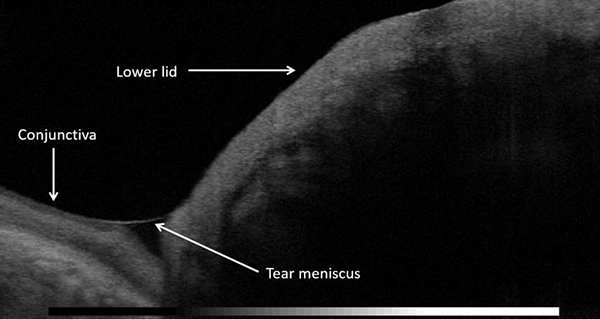
Measuring the inferior tear meniscus height (meniscometry) will give an indication of tear volume (Figure 3). This is simple and quick to perform and can easily form part of any anterior eye examination, but is especially important during the pre-assessment of potential contact lens wearers.
To measure tear prism height, an illuminated slit set horizontally in alignment with the lower lid margin can be altered until it appears to match the height of the tear prism (Figure 3).

A value in millimetres can be obtained by using a horizontal slit beam and adjusting the slit width to match the tear meniscus height centrally along the lower lid. Guillon6 proposes a clinical routine to incorporate the measurement of the tear film prism height in these positions, enabling a more comprehensive assessment of tear volume:
- Immediately below the pupil centre
- 5mm nasally
- 5mm temporally.
It is generally accepted that a tear meniscus in normal eyes measures between 0.2 and 0.4mm7.
The above method of meniscometry depends on observer reliability, and therefore repeatability of results can vary. Newer instruments may allow a more accurate method of measuring the tear meniscus using integrated calipers and has been shown to have accuracy of 0.1mm.8 Optical Coherence Tomography (OCT), now widely available in optometric practice, has been recognised by the DEWS II Methodology report as a quick and simple way to measure tear meniscus height (Figure 4). Although it recognises that further development of validated measurement software is needed it recognises that it has shown to have good intra-observer and inter-observer repeatability.
Although less commonly used in clinical practice, alternative invasive techniques for measuring tear volume include the Schirmer test and the Phenol red thread test.
(b) the tear meniscus height using integrated calipers
The Schirmer test involves hooking an absorbent tear test strip of paper over the margin of the lower lid (Figure 5). The length of wetting from the bend is measured in millimetres after five minutes. A normal tear film should produce a wetting length of more than 10mm. Dry eye is indicated where there is less than 5mm of wetting.10 The invasive nature of this technique results in excessive reflex tearing, limiting the value of the test in clinical practice.
There appears to be a reluctance to discard this test, which is partly due to the fact that it is still the simplest, fastest and least expensive diagnostic test available for assessing tear production.
DEWS II, whilst recognising that the variability and invasiveness of the Schirmer test precludes it as a diagnostic test of tear quantity, recommended it as a test to confirm severe aqueous deficiency in conditions such as Sjögren’s syndrome.
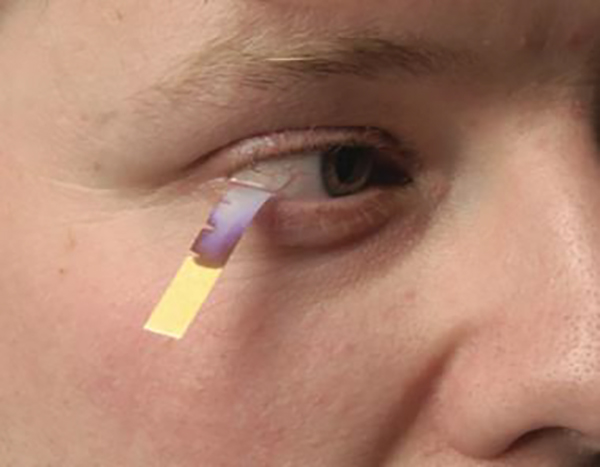
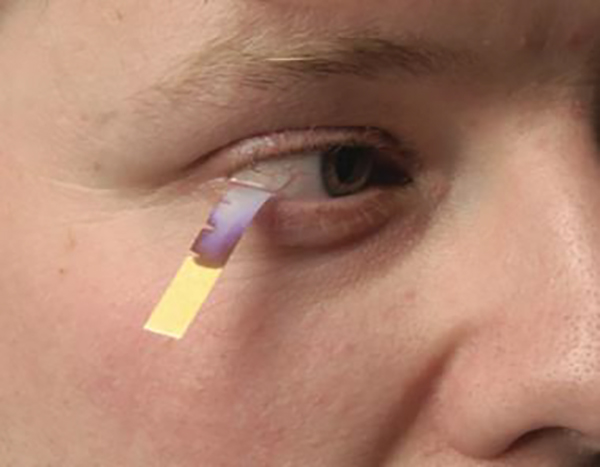


The Phenol red thread test has the advantage of being less invasive than the Schirmer test, utilising a two-ply cotton thread impregnated with phenol red dye.
Phenol red is pH sensitive and changes from yellow to red when wetted by tears, due to the alkaline nature of tears (pH 7.6).9 The length of the colour change on the thread, indicating the length of the thread wetted by the tears, is measured in millimetres.
Wetting lengths should normally be between 9mm and 20mm. Values of less than 9mm have been shown to correlate with subjective symptoms of dryness. DEWS II Methodology recognise the Phenol Red test as a realistic measurement of resting tear volume.10
(To be continued in the next article)
Author: Marie-Therese Hall*
Editor: Rachel Hiscox*
*Marie-Therese Hall is an Optometrist and a paid consultant faculty member for the Johnson & Johnson Institute, UK and a Professional Affairs Consultant for Johnson & Johnson Vision.
Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies.
This article was produced without further input or review from the original authors.
References:
https://visionplusmag.com/j-j-references