Corneal topography is an indispensable tool in the diagnosis and treatment of various eye conditions…
Assessing the curvature of the cornea is a very crucial tool in the diagnosis and treatment of a number of conditions, or while planning refractive surgery such as LASIK and the evaluation of its results. It is also a valuable tool in the fitting of contact lenses and for orthokeratology treatment.
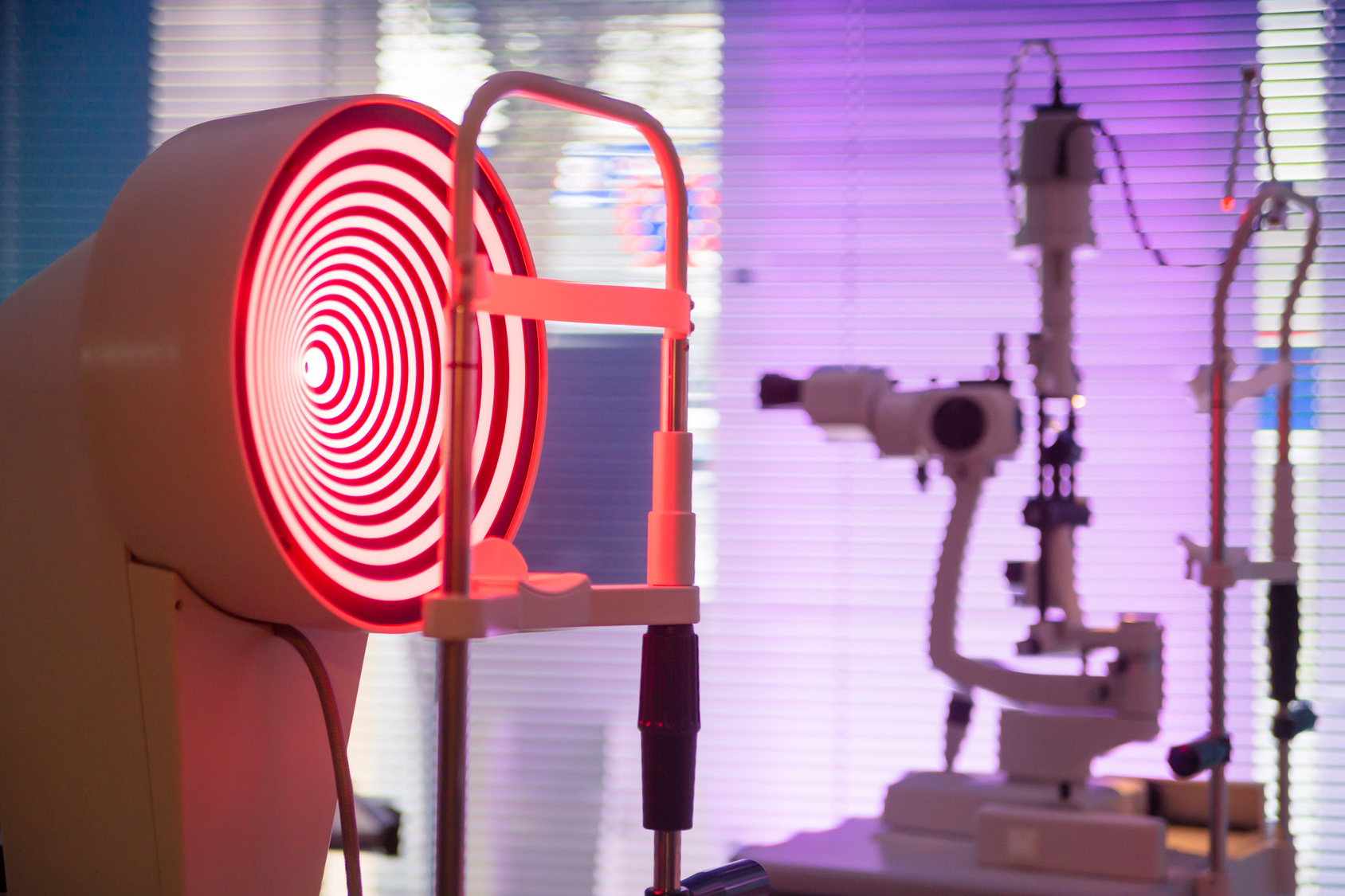
While several methods of measuring the corneal shape have been in existence, the most common tool is the keratometer. However, keratometry has the limitation of measuring the corneal curvature from only two points, approximately 3 mm apart. Other instruments using a bull’s-eye pattern reflected off the cornea have been used for years to obtain a qualitative evaluation of the corneal shape over a large area. With the introduction of computer-assisted topographical analysis, the bull’s-eye concept has been used to get more quantifiable data and more accurate visualization of the shape of the cornea. The topographer, as the name implies, maps the entire cornea.
Corneal topography is also known as Photokeratoscopy or Videokeratography. It is a non-invasive medical imaging technique used for mapping the surface curvature of the cornea. Since the cornea is normally responsible for approximately 70% of the eye’s refractive power, its topography is of critical importance in determining the quality of vision.
A development of keratoscopy, corneal topography extends the measurement range from the four points a few millimeters apart that is offered by keratometry to a grid of thousands of points covering the entire cornea. It provides a three-dimensional map, which is a valuable aid to the examining ophthalmologist or optometrist. It is used in diagnosing certain types of problems, in evaluating a disease’s progression, in fitting some types of contact lenses, and in planning surgery. It is commonly used while preparing for refractive eye surgery.
The corneal topography map is used in conjunction with other tests to determine exactly how much corneal tissue will be removed to correct the visual defect.
How corneal topography works
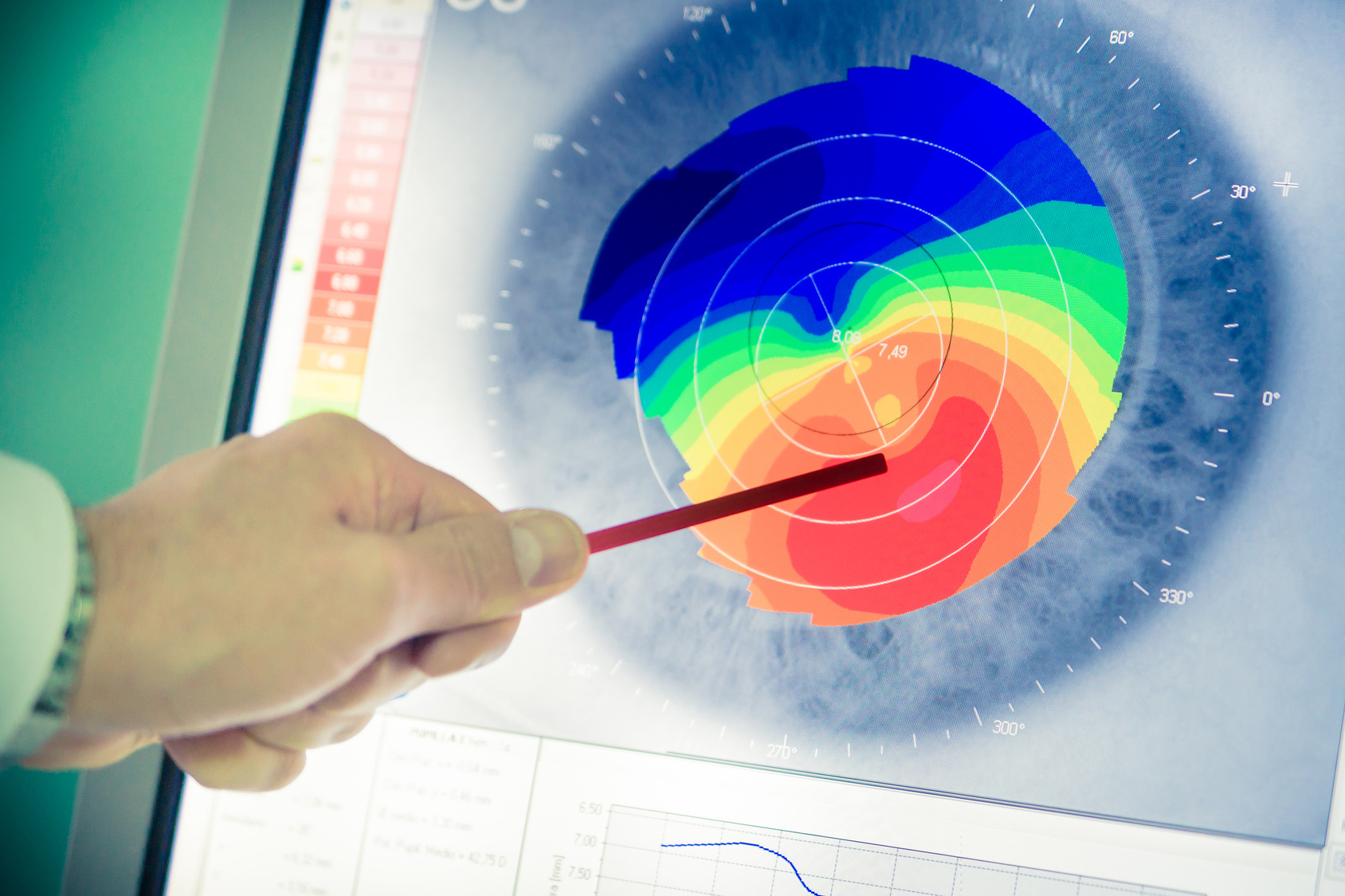
The corneal topographer comprises a computer linked to a lighted bowl, which contains a pattern of concentric rings. The patient is asked to sit in front of the bowl with his/ her head pressed against a bar. Multiple light concentric rings are then projected on the cornea and the reflected image is captured on charge-coupled device (CCD) camera. The computer software then digitizes these data points and prints out the corneal shape, using different colours to identify different elevations. The cool shades of blue and green are used to indicate flatter areas of the cornea, while warmer shades of orange and red indicate steeper areas. This map of the cornea allows the physician to formulate a 3D perspective of the cornea’s shape.
The greatest advantage of corneal topography is its ability to detect conditions invisible to most conventional testing.
Uses of corneal topography
Corneal topography is used in the diagnosis and management of various corneal curvature abnormalities and diseases such as:
- Keratoconus: This is a degenerative condition that causes a thinning of the cornea. The visual disturbance caused by keratoconus is mainly due to the irregular shape of the corneal surface. In order to effectively follow the progression of the disease and to fit a keratoconus cornea with contact lenses it is helpful to know the precise shape of the cornea.
- Corneal transplants: During such transplants an ophthalmologist replaces donor cornea to recipient cornea. After the procedure to detect the correct analysis of visual acuity and required prescription it is necessary to know the amount of cylindrical correction, which in turn becomes difficult with use of the keratometer.
- Corneal scars, Corneal deformities or opacities: Corneal scars are more likely to induce irregular astigmatism. Topography values help in RGP contact lens fitting.
- Fitting contact lenses: The use of corneal topography in clinical practice is seen in the fitting of gas permeable lenses. Corneal topography is also used in the yearly analysis of corneal changes in soft contact lens patients. It is also mandatory in corneal reshaping (orthokeratology) in monitoring corneal changes.
- Irregular astigmatism following corneal transplantation: Corneal topography helps to know the diopteric value of corneal astigmatism and in which meridian. So, it helps an ophthalmologist to know where to release the suture after the surgery for better potential visual acuity of the patient
- Refractive surgery: Topography is an important diagnostic procedure to plan LASIK and PRK procedures. Post refractive surgery, topography readings also assist to plan management.
- Postoperative cataract extraction with acquired astigmatism: There are few surgeries done by taking sutures which induces some amount of astigmatism. This can resolves once the sutures are removed.