This post is also available in:
![]() العربية
العربية
The new study is based on the analysis of a corneal transplantation unaffected for donor corneas preserved for 11 days, expanding pool of available tissue
According to a study conducted by the National Institutes of Health, the corneal donor tissue can be stored for eleven days. Experts at NIH arrived at this conclusion after studying the success of transplantation surgery to restore vision in people with disease of the cornea/ The corneal tissue used in this transplant had been stored for eleven days. Results from a large, national clinical trial show that corneal donor tissue can be safely stored for 11 days without negatively impacting the success of transplantation surgery to restore vision in people with diseases of the cornea. The cornea is the eye’s clear outer covering. Currently, donor corneas are generally not used for surgery in the United States if they have been preserved for longer than seven days.
Expanding the window in which donor tissues can be considered suitable by even just a few days should help safeguard quality donor tissue and access to vision-saving transplantation procedures. The study’s lead investigator was Jonathan Lass, M.D., of Case Western Reserve University School of Medicine and University Hospitals Eye Institute, Cleveland. Patients were randomly assigned to one of two treatment groups. The first received corneas preserved up to seven days, and the second received corneas preserved for eight to 14 days.
The U.S. Food and Drug Administration has approved the use of solutions to preserve donated corneas for 14 days. “The current practice of surgeons to use corneas preserved for no longer than seven days is not evidence-based,” said Lass. However, he is hopeful that this practice based on opinion will change in the light of new evidence.
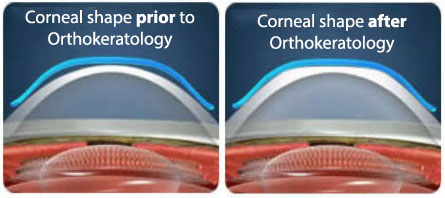
In this cross section of a cornea in a person with Fuchs’ dystrophy, the green rectangles represent endothelial cells. The magenta dots are outgrowths of Descemet’s membrane known as guttae. Guttae are bumps on the back surface of the cornea that grow larger as the disease progresses. During DSAEK, Descemet’s membrane and the endothelium are stripped away.
Two reports from the Cornea Preservation Time Study (CPTS), which was funded by the National Eye Institute, part of the National Institutes of Health, appear online Nov. 10 in JAMA Ophthalmology.
Researchers looked at three-year graft success rates among a total of 1,090 individuals (1,330 eyes) who underwent transplantation via Descemet’s stripping automated endothelial keratoplasty by 70 surgeons at 40 surgical sites. Most of the patients underwent transplantation for Fuchs’ endothelial corneal dystrophy, a progressive disease that causes cells to die in the innermost layer of the corneacalled the endothelium. Death of corneal endothelial cells is a normal part of aging. However, Fuchs’ accelerates this cell death. In such cases, corneal transplantation is the only treatment available to restore vision.Overall, the investigators were unable to conclude that three-year success rates were the same for corneas preserved for eight to 14 days compared with up to seven days (92.1 percent versus 95.3 percent). However, parsing out the data, they found that much of the difference between the groups was accounted for by those who received corneas preserved 12 to 14 days. There was no meaningful difference between those who received corneas preserved up to seven days and those who received corneas preserved eight to 11 days.
While it is true that patients who received corneas preserved 12 to 14 days had comparably lower success rates, Dr. Lass emphasized that even their success was impressively high at 89.3 percent, which may support the use of these tissues as logistics dictate.
In a separate analysis of the data, the investigators analyzed the extent of endothelial cell loss (ECL), that is, the loss of cells in the corneal endothelium that continued to occur as a normal part of aging in the grafted donor cornea three years after it had been transplanted. They looked to see if differences in corneal preservation time affected ECL after three years. They noninvasively measured ECL in the 945 eyes with successful grafts and found that corneas preserved up to seven days had a 37-percent loss of cells versus a 40-percent loss in corneas preserved eight to 14 days. However, taking a closer look at the data revealed that the effect of corneal preservation time on the loss of endothelial cells was comparable from four to 13 days.
Taken together, the separate analyses looking at graft success rates and ECL support the use of corneas stored up to 11 days.
Currently, there is a sufficient supply of donor corneas available for people in the United States who require transplants. In 2016, nearly 50,000 corneal transplantations were performed and, on average, it took only about three to four weeks for donor tissue from an eye bank to become available for scheduled surgery. However, corneal donor tissue is scarce elsewhere in the world and corneal disease is the third leading cause of blindness outside the U.S.
“Additionally, factors balancing supply and demand in the U.S. may shift unfavorably as the population with age-related diseases of the cornea grows, and the supply of donors is challenged by the increasing prevalence of conditions in deceased donors that make their corneas ineligible for donation,” said study investigator Marian Macsai, M.D., an ophthalmologist at NorthShore University Health System, Glenview, Illinois, and president of the Cornea Society, a U.S.-based international society of corneal surgeons. Prior to transplantation, tissue from a donor must be rigorously screened for safety and viability. That means ruling out certain infectious and communicable diseases in the donor.
This new finding is expected to play a crucial role in expanding the donor pool for corneal transplants. Two reports from the Cornea Preservation Time Study (CPTS), which was funded by the National Eye Institute, part of the National Institutes of Health detailing the investigation and conclusion also appear online in the JAMA Ophthalmology journal.
The research was supported by grants from NEI EY20797 and EY20798.
Credits:
National Institutes of Health
Rosenwasser, O. George, “Effect of Cornea Preservation Time on Descemet Stripping Automated
Endothelial Keratoplasty Success: Results of a Randomized Non-Inferiority Trial.” JAMA Ophthamol. Published online Nov. 10, 2017. DOI:10.1001/jamaophthalmol.2017.4989
Lass, H. Jonathan, “Corneal Endothelial Cell Loss 3 Years After Successful Descemet Stripping Automated
Endothelial Keratoplasty in the Corneal Preservation Time Study.” JAMA Ophthamol. Published online Nov. 10, 2017. DOI:10.1001/jamaophthalmol.2017.4970